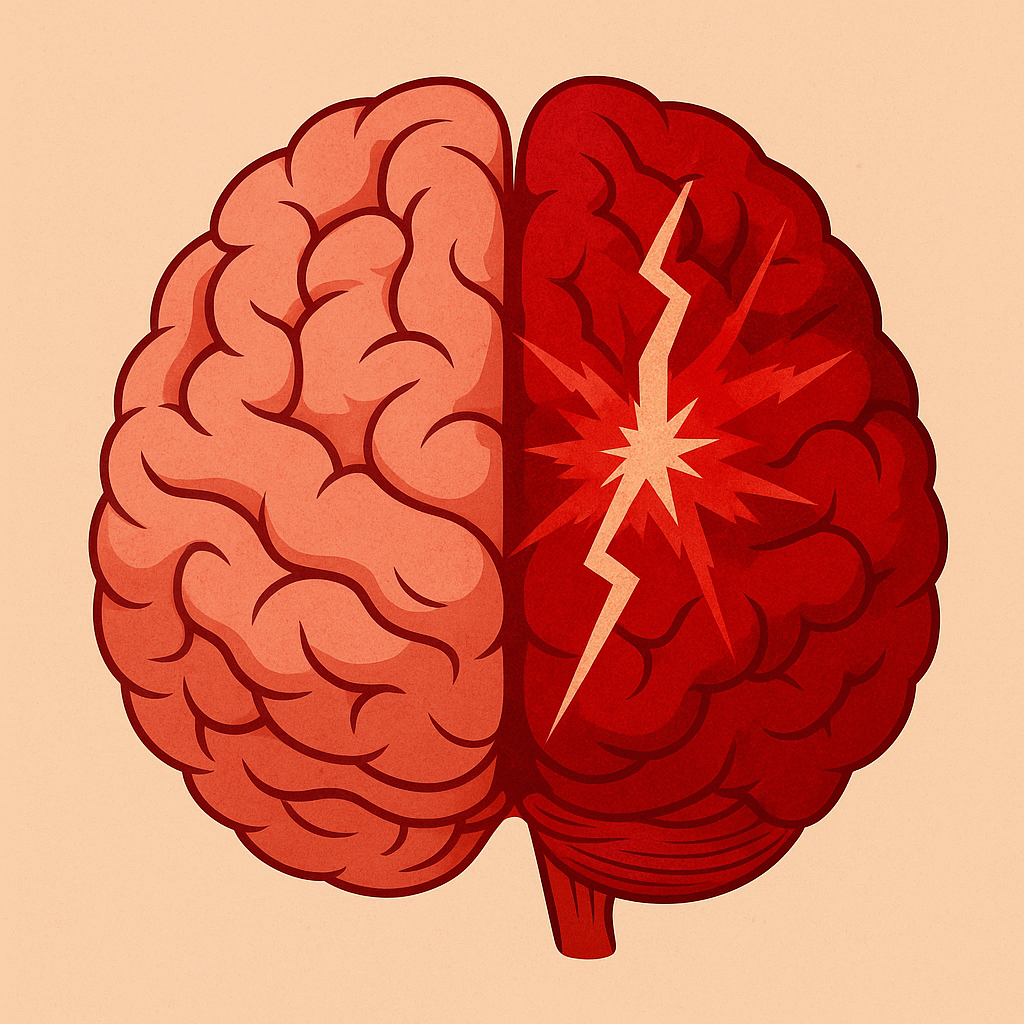
What is Stroke and how can we recover from it?
A stroke happens when blood flow to the brain is blocked or a blood vessel bursts, cutting off the oxygen and nutrients the brain needs. This can cause sudden symptoms like weakness or numbness on one side of the body, slurred speech, trouble understanding, vision changes, dizziness, or a severe headache. Getting medical help quickly is critical, as brain damage starts within minutes. After a stroke, some people may face challenges such as weakness, movement or balance problems, speech or swallowing difficulties, changes in memory or thinking, or shifts in mood. But recovery is possible with the right care and support, many stroke survivors regain strength, skills, and independence. Rehabilitation such as physiotherapy plays a vital role in helping the brain and body relearn, adapt, and keep improving over time, giving survivors the best chance to return to a fulfilling and active life.
How does stroke affect your daily life?
Common physical impairments after a stroke:
- Weakness or paralysis (often on one side of the body — arm, leg, or face)
- Loss of coordination and balance, making walking or daily activities difficult due to ataxia and other disordered movements.
- Increased muscle tone, stiffness or spasticity, leading to tightness or involuntary movements
- Reduced range of motion in joints or limbs
- Difficulty with fine motor skills, such as writing, buttoning clothes, or using utensils
- Swallowing problems (dysphagia), which may affect eating and drinking safely
- Speech and language difficulties (dysarthria/aphasia), which can overlap with cognitive impairments but often stem from muscle weakness or control issues
- Fatigue, which may be physical (low endurance, easily tired)
- Visual changes, such as double vision, partial loss of vision, or difficulty focusing
- Sensory changes, like numbness, tingling, or altered sensation
After a stroke, some people may find everyday activities like walking, dressing, cooking, or driving more challenging, and may step back from work, hobbies, or social gatherings. Communication or memory changes can also affect conversations and community involvement. While these restrictions can feel overwhelming at first, with physical therapy and rehabilitation many stroke survivors regain independence, rejoin social and family life, and return to the activities that are most meaningful to them.
How can physiotherapy help stroke patients?
Neuroplasticity
Encourages brain rewiring (neuroplasticity) – repetitive, guided movements that help the brain form new pathways for control.
Restores movement and strength – exercises to improve muscle power and flexibility, especially on the weaker side of the body.
Repetition with feedback – movements are repeated many times, with the therapist giving immediate feedback, so the brain builds stronger connections through neuroplasticity.
Task-oriented practice – applying these techniques to everyday activities like reaching for objects, stepping forward, or standing up, so improvements translate into daily life.
Neuromuscular Facilitation Techniques
Retrains walking – gait training to help patients walk more safely and independently.
Guided movement patterns – the therapist uses their hands to guide a patient’s arms, legs, or trunk through smooth, controlled movements, helping the brain relearn normal movement patterns.
Sensory stimulation – touch, tapping, or stretching may be used to “wake up” weak or inactive muscles and encourage them to contract.
Encouraging symmetry – helping patients use their weaker side alongside their stronger side to avoid over-reliance on one half of the body.
Weight-bearing activities – positioning a weak arm or leg to take weight (such as leaning on the hands or standing with support) helps activate muscles and improve awareness of that limb.
Enhances mobility in daily life – practicing tasks like standing up from a chair, climbing stairs, or reaching for objects.
Spasticity Management
Reduces stiffness, spasticity and prevents contractures – stretching, positioning, and movement techniques to ease tightness in muscles.
Weight-bearing and functional postures – encouraging the affected limb to support weight (e.g., leaning through the arm, standing with even weight on both legs) to help relax overactive muscles.
Splints and supports – sometimes using braces, splints, or cushions to maintain proper alignment, prevent contractures, and make daily tasks easier.
Cardiovascular Training
Reducing risk of another stroke – improving cardiovascular health lowers blood pressure, cholesterol, and helps manage weight, all of which reduce recurrence risk.
Boosting overall well-being – aerobic exercise also improves mood, energy levels, and confidence, supporting mental health in recovery.
Promoting independence – better cardiovascular fitness makes it easier to return to work, hobbies, and social activities.
Balance and Coordination Training
Improves balance and coordination – training to reduce the risk of falls and increase confidence in moving around.
Gait retraining for ataxia – breaking walking down into smaller, controlled steps, often using visual or tactile cues (like stepping over markers on the floor) to reduce unsteady, jerky movements.
Postural control training – supporting the trunk and core muscles to improve sitting, standing, and balance control.
What should I do next?
Physiotherapy plays a vital role in the recovery and management of stroke survivors. With regular and timely rehabilitation, you can prevent complications such as joint contractures, muscle weakness, or loss of function from inactivity and promote independence by regaining mobility and functional movements such as walking and standing. Reach out to us and let us help you on your rehabilitation journey!
